Hammer Toe Fusion Implant
When a person has Hammer toe, the end of their toe hammertoe bends downward and the middle joint curls up. Eventually, the toe gets stuck in a stiff, claw-like position. When the inside of your shoe rubs against a hammer toe, corns, blisters or calluses may form on top of the toe or on the bottom of your foot. This can make walking painful. You may also have pain in the joint where your big toe joins your foot. Hammer toe usually affects a person?s second toe (the toe next to the big toe), but it can affect other toes too.
Causes
The muscles of each toe work in pairs. When the toe muscles get out of balance, a hammertoe can form. Muscle imbalance puts a lot of pressure on the toe's tendons and joints. This pressure forces the toe into a hammerhead shape. How do the toe muscles get out of balance? There are three main reasons. Genes. you may have inherited a tendency to develop hammertoes because your feet are somewhat unstable, they may be flat or have a high arch. Arthritis. Injury to the toe, ill-fitting shoes are the main culprits. If shoes are too tight, too short, or too pointy, they push the toes out of balance. Pointy, high-heeled shoes put particularly severe pressure on the toes.
 Symptoms
Symptoms
The most obvious symptom of hammertoe is the bent, hammer-like or claw-like appearance of one or more of your toes. Typically, the proximal joint of a toe will be bending upward and the distal joint will be bending downward. In some cases, both joints may bend downward, causing the toes to curl under the foot. In the variation of mallet toe, only the distal joint bends downward. Other symptoms may include Pain and stiffness during movement of the toe, Painful corns on the tops of the toe or toes from rubbing against the top of the shoe's toe box, Painful calluses on the bottoms of the toe or toes, Pain on the bottom of the ball of the foot, Redness and swelling at the joints. If you have any of these symptoms, especially the hammer shape, pain or stiffness in a toe or toes, you should consider consulting your physician. Even if you're not significantly bothered by some of these symptoms, the severity of a hammertoe can become worse over time and should be treated as soon as possible. Up to a point hammertoes can be treated without surgery and should be taken care of before they pass that point. After that, surgery may be the only solution.
Diagnosis
Most health care professionals can diagnose hammertoe simply by examining your toes and feet. X-rays of the feet are not needed to diagnose hammertoe, but they may be useful to look for signs of some types of arthritis (such as rheumatoid arthritis) or other disorders that can cause hammertoe. If the deformed toe is very painful, your doctor may recommend that you have a fluid sample withdrawn from the joint with a needle so the fluid can be checked for signs of infection or gout (arthritis from crystal deposits).
Non Surgical Treatment
Hammertoes that are not painful (asymptomatic) and still flexible may not require treatment. In mild cases, open-toed, low-heeled, or wider shoes and foam or moleskin pads can provide symptomatic relief by reducing pressure. Taping (strapping) the affected toe can help to reduce deformity and pain. Physical therapy to instruct patients in exercises that passively stretch tight structures and strengthen weak foot intrinsic muscles is also helpful with mild cases. Periodic trimming (debridement) of corns (clavi, helomata) by a podiatrist can provide temporary relief. Corticosteroid injections are often very effective in reducing pain.
Surgical Treatment
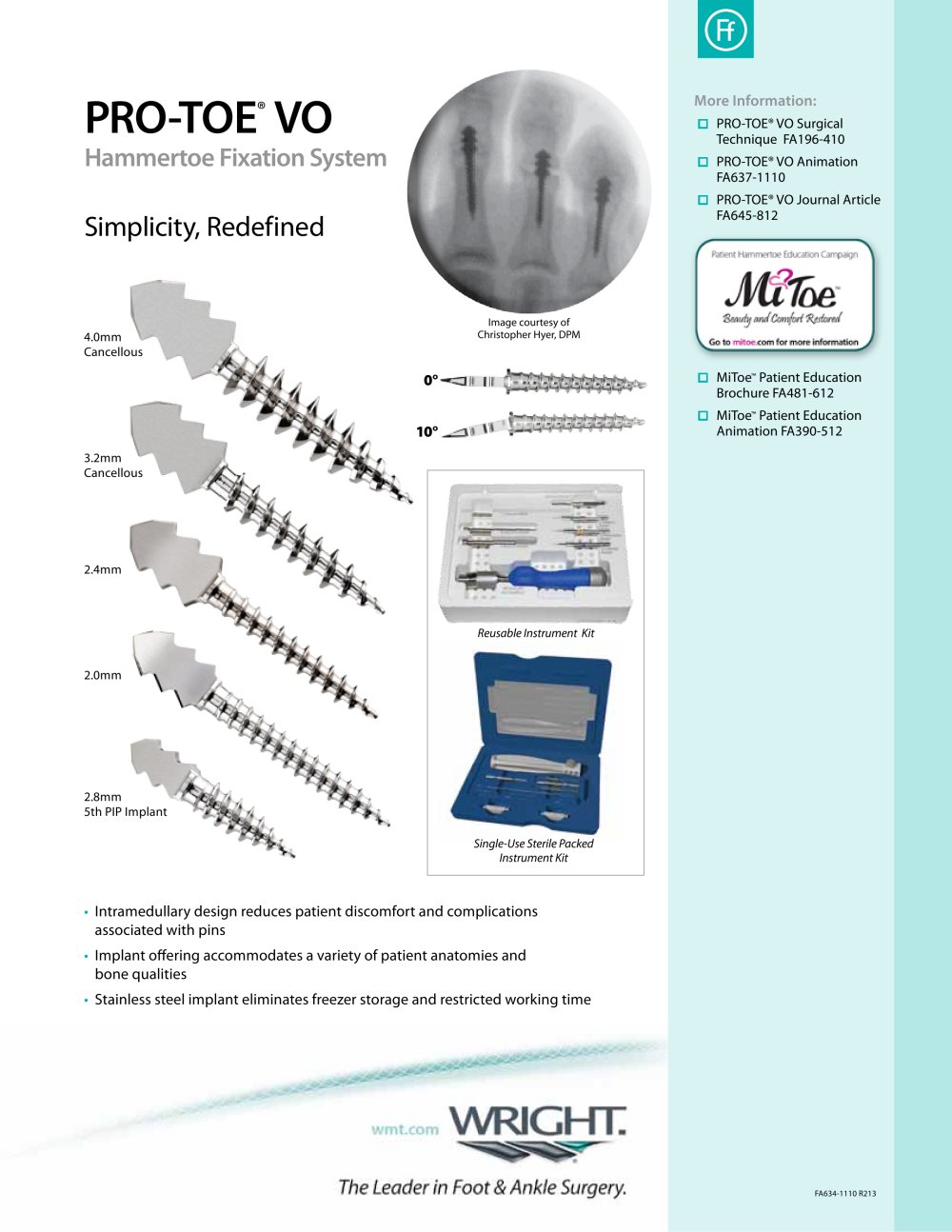
There are several surgical methods to correct a hammer toe. Your physician will decide which method will be most beneficial to you depending on the severity of your deformity, the direction the toe is deviating and the length of the affected toe. Some common surgical methods include. Arthroplasty. To promote straightening, half of the joint located directly underneath the crooked part of the toe is removed. Arthrodesis (fusion) To promote straightening, the joint directly underneath where the toe is crooked is completely removed. A wire or pin is inserted to aid healing. Tendon transfer. Performed alone or in combination with other procedures, a surgeon will take tendons from under the toe and ?re-route? them to the top of the toe to promote straightening. Basal phalangectomy. Performed to assist patients with severe stiffness, this procedure removes the base of the bone underneath the toe. Weil osteotomy. Performed to assist patients with severe stiffness, this procedure involves shortening the metatarsal bone and inserting surgical hardware to aid healing.
Hammer Toe Pain
 Overview
Overview
When there?s an imbalance in the muscle and ligament surrounding a toe joint, the effect is a bend in the middle joint of the toe, which causes the whole toe to bend upward. Because the toe is bent in an unnatural way, it?s common for the toe to become irritated and even develop corns. A toe that curls under rather than bends upward is also considered a hammertoe.
Causes
While there are a number of causes, there aren't many specific risk factors for hammertoes, women tend to get these problems more than men, but they occur without rhyme or reason. Diabetics, however, are more likely to get a hammertoe if they have underlying nerve damage in the toes and feet.
 Symptoms
Symptoms
A soft corn, or heloma molle, may exist in the web space between toes. This is more commonly caused by an exostosis, which is basically an extra growth of bone possibly due to your foot structure. As this outgrowth of excessive bone rubs against other toes, there is friction between the toes and a corn forms for your protection.
Diagnosis
First push up on the bottom of the metatarsal head associated with the affected toe and see if the toe straightens out. If it does, then an orthotic could correct the problem, usually with a metatarsal pad. If the toe does not straighten out when the metatarsal head is pushed up, then that indicates that contracture in the capsule and ligaments (capsule contracts because the joint was in the wrong position for too long) of the MTP joint has set in and surgery is required. Orthotics are generally required post-surgically.
Non Surgical Treatment
Treating hammertoe involves straightening the toe, making tendons in the toes flexible again, and preventing the problem from returning. Some simple treatments include splinting the toe to keep it straight and to stretch the tendons of the foot. Using over-the-counter pads, cushions or straps to decrease discomfort Exercising the toes to relax the foot tendons (a session with a physical therapist may help you get started with foot exercises) Wearing shoes that fit properly and allow toes plenty of room to stretch out.
Surgical Treatment
Treatment of a severe hammertoe that has become rigid includes surgery. What is done during the surgery depends on how misshapen and inflexible the toe is. The surgeon may make a cut over your toe and release the tendon by cutting the tendon away from the bone. The surgeon may remove a small piece of bone from the toe. The surgeon may realign the tendons to reposition your toe or fasten the bones with hammertoes pins. Sometimes the surgeon may have to join the bones in the toe. In this case, you will no longer be able to bend the toe, but the toe will be flat.
 Prevention
Prevention
These tips may help you buy the right shoes. Buy shoes at the end of the day. Your feet are smaller in the morning and swell throughout the day. Don't assume your shoe size hasn't changed. As you age, your shoe size may change, especially the width. Measure both feet and buy for the larger foot. Ask for just the right fit. A shoe repair store can stretch shoes in tight spots.
Bunions Foot Pain
Overview
 Bunions (hallux valgus) are often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. With a bunion, the big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment, producing the bunion's "bump." Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which continues to become increasingly prominent. Bunions can be painful, but not always. Bunions are always progressive, so the deformity becomes more prounced over time, even if its not painful.
Bunions (hallux valgus) are often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. With a bunion, the big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment, producing the bunion's "bump." Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which continues to become increasingly prominent. Bunions can be painful, but not always. Bunions are always progressive, so the deformity becomes more prounced over time, even if its not painful.
Causes
The commonest cause of bunions is prolonged wearing of poorly designed shoes such as the narrow high heels that women wear. This is one of the reasons why bunions are much more common in women than in men. There is also a hereditary component to bunions in that many times we will see a grandmother, mother and daughter all with various stages of bunions. 38% of women in the United States wear shoes that are too small and 55% of women have some degree of bunion formation. Bunions are 9 times more common in women than they are in men.
Symptoms
Symptoms often include pain, swelling, and abnormal position of the first toe. The technical term for bunions is ?hallux valgus? (HV). This refers to the first toe or hallux moving away or abducting from the middle of the foot and then twisting in such a way that the inside edge actually touches the ground and the outside edge turns upward. This term describes the deviation of the toe toward the outside part of the foot. If left untreated, bunions can worsen over time and cause considerable difficulty in walking, discomfort, and skin problems such as corns. In some cases, a small bursa (fluid-filled sac) near the joint becomes inflamed. This condition is known as bursitis and can cause additional redness, swelling, and pain. Less frequently, bunions occur at the base of the fifth toe. When this occurs, it is called a ?tailor?s bunion? or bunionette.
Diagnosis
Your doctor is very likely to be able to diagnose your bunion simply by examining your foot. Even before that, he or she will probably ask about your family and personal medical history and evaluate the types of shoes you wear. You'll be asked about your symptoms, when they started and when they occur. You may also be asked to flex your toe so that your doctor can get an idea of your range of motion. He or she may order x-rays in order to determine the extent of your deformity.
Non Surgical Treatment
Wear comfortable shoes that don't squeeze your toes together. Sandals are ideal in warm weather. Cushioning the bunion with a donut-shaped bunion pad sold at drugstores can prevent any direct rubbing against your shoes. Have your shoes stretched to give your foot more room or consider switching to footwear customized to relieve pressure on the affected area. Soak your foot in warm water to help lessen the pain after a day on your feet. Apply ice packs several times a day to reduce swelling of painful and inflamed bunions. Take aspirin or ibuprofen for the inflammation and pain, and try supplementing with anti-inflammatory herbs such as ginger and turmeric (these work more slowly than the drugs). See a podiatrist for specially fitted shoes or orthotic devices that may help. Sometimes, surgery is necessary. Seek a second opinion before scheduling any operation. 
Surgical Treatment
If these methods fail, then surgery may be suggested. Basically, bunion surgery is performed to improve function or to prevent pain from occurring. When surgery is delayed in a symptomatic foot, greater amounts of arthritis can develop and the more complicated surgery can become. Surgery is performed to improve alignment and function to the big toe joint. The large bump is removed and, sometimes, a cut is made into the bone, to move it to a more normal position. Screws, pins and wires can be used beneath the skin, to improve healing and results. Healing can range from 3-12 weeks, depending on the procedure.
Over-Pronation
Feet are supposed to roll inward as a part of every step you take. This helps them to mold to the various terrain that they step on (sand, rocks, various obstacles) without injury. This is called pronation. But, when your feet roll inward excessively, problems often arise. Excessive inward rolling of the feet and ankles is called over-pronation. Sometimes, people who over-pronate are told they have ?flat feet?. The term ?flat feet? can be misleading. When standing, body weight causes the arch of most feet to flatten out somewhat. This does not mean they become flat like pancakes (though some feet do). Instead, the arch shape gets longer and flatter and the arch height gets lower.

Causes
Excess stress on the inner surface of the foot can cause injury and pain in the foot and ankle. Repeated rotational forces through the shin, knee, thigh and pelvis also place additional strain on the muscles, tendons and ligaments of the lower leg.
Symptoms
Because pronation is a twisting of the foot, all of the muscles and tendons which run from the leg and ankle into the foot will be twisted. In over-pronation, resulting laxity of the soft tissue structures of the foot and loosened joints cause the bones of the feet shift. When this occurs, the muscles which attach to these bones must also shift, or twist, in order to attach to these bones. The strongest and most important muscles that attach to our foot bones come from our lower leg. So, as these muscles course down the leg and across the ankle, they must twist to maintain their proper attachments in the foot. Injuries due to poor biomechanics and twisting of these muscles due to over-pronation include: shin splints, Achilles Tendonitis, generalized tendonitis, fatigue, muscle aches and pains, cramps, ankle sprains, and loss of muscular efficiency (reducing walking and running speed and endurance). Foot problems due to over-pronation include: bunions, heel spurs, plantar fasciitis, fallen and painful arches, hammer toes, and calluses.
Diagnosis
At some point you may find the pain to much or become frustrated. So what are you options? Chances are your overpronation has led to some type of injury if there's pain. Your best bet is to consult with someone who knows feet. Start with your pediatrist, chiropodist or chiropractor. They'll be able to diagnose and treat the injury and give you more specific direction to better support your feet. One common intervention is a custom foot orthotic. Giving greater structural support than a typical shoe these shoe inserts can dramatically reduce overpronation.

Non Surgical Treatment
Supportive orthotics in the shoe is a method commonly implemented to treat many common running injuries associated with pronation. An advantage of orthotics is that they often allow the sufferer to continue to participate in athletic activity and avoid other treatment options that could be potentially costly and time consuming. Seventy-five percent of injured runners are successfully treated with the prescription of orthoses. Orthotics are the most effective treatment for symptoms that develop from unusual biomechanics within the body such as overpronation, resulting in either great improvement or complete healing of the injury in about half the cases.
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
Can I Care For Severs Disease In The Home?
Severs disease is by far the most common cause of heel pain in young children, the condition commonly occurs in kids around the age of 10-15 years. Severs is a traction apophysitis in which inflammation of the calcaneal apophysis (growth plate) occurs as a result of overuse or micro trauma. As mentioned severs disease is caused by micro trauma and over use, this can include excessive foot pronation (foot rolling in), tight calf muscles, increase in sporting activities and inappropriate footwear. These all put extra sheering forces on the growth plate leading to aggravation and resultant pain. Signs and symptoms of this include pain on squeezing of the heel, absence of swelling and redness, child describing pain as a dull ache, limping and pain with increased activity.
Causes
Having flatfeet or very pronated feet can make one prone to Sever's disease. But also patient?s that have a very high arch foot structure tend to have a very high shock and high impact heel strike. This also puts extra stress on the heel and apophysis.
Symptoms
The most prominent symptom of Sever?s disease is heel pain which is usually aggravated by physical activity such as walking, running or jumping. The pain is localised to the posterior and plantar side of the heel over the calcaneal apophysis. Sometimes, the pain may be so severe that it may cause limping and interfere with physical performance in sports. External appearance of the heel is almost always normal, and signs of local disease such as edema, erythema (redness) are absent. The main diagnostic tool is pain on medial- lateral compression of the calcaneus in the area of growth plate, so called squeeze test. Foot radiographs are usually normal. Therefore the diagnosis of Sever?s disease is primarily clinical.
Diagnosis
In Sever's disease, heel pain can be in one or both heels. It usually starts after a child begins a new sports season or a new sport. Your child may walk with a limp. The pain may increase when he or she runs or jumps. He or she may have a tendency to tiptoe. Your child's heel may hurt if you squeeze both sides toward the very back. This is called the squeeze test. Your doctor may also find that your child's heel tendons have become tight.
Non Surgical Treatment
Once diagnosed, there is a list of treatment options available to begin the recovery process. Unfortunately due to the nature of the condition it will often be a reoccurring condition until closure of the growth plates of the heel and elongation of the soft tissue structures. However with appropriate education, correct management of symptoms and prevention strategies, Severs disease can be well managed by the individual and their parents.
Flat Foot Problems In Adults
Overview
Adult-acquired flatfoot is a challenging condition to treat. It is defined as a symptomatic, progressive deformity of the foot caused by loss of supportive structures of the medial arch. It is becoming increasingly frequent with the aging population and the obesity epidemic. Patients commonly try to lose weight by exercising to improve the condition. This often leads to worsening of symptoms and progression of the disorder. Early recognition of this complex disorder is essential, if chronic pain and surgery are to be avoided. 
Causes
Obesity - Overtime if your body is carrying those extra pounds, you can potentially injure your feet. The extra weight puts pressure on the ligaments that support your feet. Also being over weight can lead to type two diabetes which also can attribute to AAFD. Diabetes - Diabetes can also play a role in Adult Acquired Flatfoot Deformity. Diabetes can cause damage to ligaments, which support your feet and other bones in your body. In addition to damaged ligaments, uncontrolled diabetes can lead to ulcers on your feet. When the arches fall in the feet, the front of the foot is wider, and outer aspects of the foot can start to rub in your shoe wear. Patients with uncontrolled diabetes may not notice or have symptoms of pain due to nerve damage. Diabetic patient don?t see they have a problem, and other complications occur in the feet such as ulcers and wounds. Hypertension - High blood pressure cause arteries narrow overtime, which could decrease blood flow to ligaments. The blood flow to the ligaments is what keeps the foot arches healthy, and supportive. Arthritis - Arthritis can form in an old injury overtime this can lead to flatfeet as well. Arthritis is painful as well which contributes to the increased pain of AAFD. Injury - Injuries are a common reason as well for AAFD. Stress from impact sports. Ligament damage from injury can cause the bones of the foot to fallout of ailment. Overtime the ligaments will tear and result in complete flattening of feet.
Symptoms
Symptoms are minor and may go unnoticed, Pain dominates, rather than deformity. Minor swelling may be visible along the course of the tendon. Pain and swelling along the course of the tendon. Visible decrease in arch height. Aduction of the forefoot on rearfoot. Subluxed tali and navicular joints. Deformation at this point is still flexible. Considerable deformity and weakness. Significant pain. Arthritic changes in the tarsal joints. Deformation at this point is rigid.
Diagnosis
In the early stages of dysfunction of the posterior tibial tendon, most of the discomfort is located medially along the course of the tendon and the patient reports fatigue and aching on the plantar-medial aspect of the foot and ankle. Swelling is common if the dysfunction is associated with tenosynovitis. As dysfunction of the tendon progresses, maximum pain occurs laterally in the sinus tarsi because of impingement of the fibula against the calcaneus. With increasing deformity, patients report that the shape of the foot changes and that it becomes increasingly difficult to wear shoes. Many patients no longer report pain in the medial part of the foot and ankle after a complete rupture of the posterior tibial tendon has occurred; instead, the pain is located laterally. If a fixed deformity has not occurred, the patient may report that standing or walking with the hindfoot slightly inverted alleviates the lateral impingement and relieves the pain in the lateral part of the foot.
Non surgical Treatment
Treatment will vary depending on the degree of your symptoms. Generally, we would use a combination of rest, immobilization, orthotics, braces, and physical therapy to start. The goal is to keep swelling and inflammation under control and limit the stress on the tendon while it heals. Avoidance of activities that stress the tendon will be necessary. Once the tendon heals and you resume activity, physical therapy will further strengthen the injured tendon and help restore flexibility. Surgery may be necessary if the tendon is torn or does not respond to these conservative treatment methods. Your posterior tibial tendon is vital for normal walking. When it is injured in any way, you risk losing independence and mobility. Keep your foot health a top priority and address any pain or problems quickly. Even minor symptoms could progress into chronic problems, so don?t ignore your foot pain. 
Surgical Treatment
Surgery is usually performed when non-surgical measures have failed. The goal of surgery is to eliminate pain, stop progression of the deformity and improve a patient?s mobility. More than one technique may be used, and surgery tends to include one or more of the following. The tendon is reconstructed or replaced using another tendon in the foot or ankle The name of the technique depends on the tendon used. Flexor digitorum longus (FDL) transfer. Flexor hallucis longus (FHL) transfer. Tibialis anterior transfer (Cobb procedure). Calcaneal osteotomy - the heel bone may be shifted to bring your heel back under your leg and the position fixed with a screw. Lengthening of the Achilles tendon if it is particularly tight. Repair one of the ligaments under your foot. If you smoke, your surgeon may refuse to operate unless you can refrain from smoking before and during the healing phase of your procedure. Research has proven that smoking delays bone healing significantly.
What Causes Heel Aches

There are two categories of Heel Pain. pain on the bottom (plantar) and pain on the back of the heel bone (calcaneus). The most common cause pain on the bottom of the heel is plantar fasciitis or better known as heel spur syndrome. Another common cause is nerve entrapment (~70% of patients have both plantar fasciitis and nerve entrapment) and less commonly, stress fracture, arthritis, tendonitis, a cyst or a combination of these. Pain on the back of the heel most often involves the insertion of the Achilles tendon into the bone. Due to the multi-factorial nature of heel pain, the earlier a diagnosis is made, the better the outcome.
Causes
Plantar fasciitis can come from a number of underlying causes. Finding the precise reason for the heel pain is sometimes difficult. As you can imagine, when the foot is on the ground a tremendous amount of force (the full weight of the body) is concentrated on the plantar fascia. This force stretches the plantar fascia as the arch of the foot tries to flatten from the weight of your body. This is just how the string on a bow is stretched by the force of the bow trying to straighten. This leads to stress on the plantar fascia where it attaches to the heel bone. Small tears of the fascia can result. These tears are normally repaired by the body. As this process of injury and repair repeats itself over and over again, a bone spur (a pointed outgrowth of the bone) sometimes forms as the body's response to try to firmly attach the fascia to the heelbone. This appears on an X-ray of the foot as a heel spur. Bone spurs occur along with plantar fasciitis but they are not the cause of the problem. As we age, the very important fat pad that makes up the fleshy portion of the heel becomes thinner and degenerates (starts to break down). This can lead to inadequate padding on the heel. With less of a protective pad on the heel, there is a reduced amount of shock absorption. These are additional factors that might lead to plantar fasciitis. Some physicians feel that the small nerves that travel under the plantar fascia on their way to the forefoot become irritated and may contribute to the pain. But some studies have been able to show that pain from compression of the nerve is different from plantar fasciitis pain. In many cases, the actual source of the painful heel may not be defined clearly. Other factors that may contribute to the development of plantar fasciitis include obesity, trauma, weak plantar flexor muscles, excessive foot pronation (flat foot) or other alignment problems in the foot and or ankle, and poor footwear.
Symptoms
Pain in the bottom of the heel is the most common symptom. The pain is often described as a knife-like, pinpoint pain that is worse in the morning and generally improves throughout the day. By the end of the day the pain may be replaced by a dull ache that improves with rest. The pain results from stretching the damaged tissues. For the same reason atheletes' pain occurs during beginning stages of exercise and is relieved over time as warm-up loosens the fascia. Plantar fasciitis onset is usually gradual, only flaring up during exercise. If pain is ignored, it can eventually interfere with walking and overall, plantar fasciitis accounts for about ten percent of all running injuries.
Diagnosis
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Most patients get better with the help of nonsurgical treatments. Stretches for the calf muscles on the back of the lower leg take tension off the plantar fascia. A night splint can be worn while you sleep. The night splint keeps your foot from bending downward. It places a mild stretch on the calf muscles and the plantar fascia. Some people seem to get better faster when using a night splint. They report having less heel pain when placing the sore foot on the ground in the morning. There have been a few studies that reported no significant benefit from adding night splinting to a program of antiinflammatory meds and stretching. Other studies report the benefits of short-term casting to unload the heel, immobilize the plantar fascia, and reduce repetitive microtrauma. Supporting the arch with a well fitted arch support, or orthotic, may also help reduce pressure on the plantar fascia. Placing a special type of insert into the shoe, called a heel cup, can reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration. Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Surgical Treatment
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
Prevention

A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don?t underestimate your body's need for rest and good nutrition. If obese, lose weight.